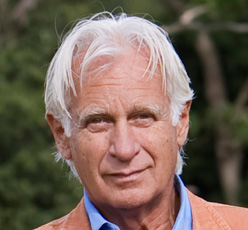
Social prescribing represents a steep learning curve for many doctors says Craig Sams, but it’s rocketing up the agenda
The setting: a GP surgery. Receptionist: “The doctor will see you now.” Doctor: “Hi, how are you getting on with your low-carb diet? Are you getting the regular exercise we agreed? Can we de-prescribe the Metformin? Let’s do a few tests to see whether you’re ready to come off the drugs. By the way, how are you getting on with your cookery classes? Let’s see if we can finally wave type 2 diabetes goodbye.”
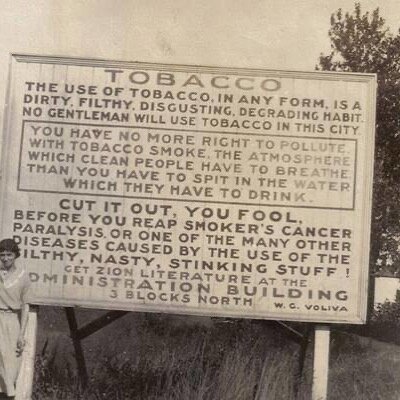
Bad news for the pharmaceutical industry but ‘social prescribing’ is on a roll and there will be a lot more of it in the future. Professor Tony Avery, the NHS National Clinical Prescribing director has said the aim is to bring about a ‘culture change’. He sees social prescribing as transforming modern healthcare, saving money and improving people’s lives. Not only that, but adverse reactions to medication are estimated to cost NHS England over £2 billion a year (not to mention the impact on people’s lives and health). The number of disability claimants doubled from 2021 to 2022. 8.3 million Britons are now on antidepressants.
The College of Medicine’s Beyond Pills Campaign is pushing hard to stop the overprescribing of medicines. The college says that 1.1 billion medicines are prescribed unnecessarily. Its chair Michael Dixon (medical advisor to King Charles), has said ‘Medicine…is no longer affordable or sustainable. A new medical mindset is needed which goes to the heart of true healthcare.”
Back in the 1930s an experiment in social prescribing called the Peckham Experiment engaged with 950 local families to get them on the track to health. They had a gym, a swimming pool, cookery classes, a vegetable garden and workshops about health. Members would have a medical health check once a year and were monitored on a regular basis. The kids did better at school, marriages were more stable and women were empowered (knitting groups helped with this). Social and community activities were organised by the members and helped reduce isolation, loneliness and alienation, illness levels fell dramatically. William Beveridge who drafted the plan for the NHS, was impressed and envisaged similar health centres up and down the country. When the Government put his plan to the British Medical Association in 1948 they were not impressed and the Government was forced to back down and agree that all ‘health services’ would solely be via the GP’s surgery. The Peckham Experiment closed down two years later.
But social prescribing is finally rocketing up the agenda. There are now 15 Pain Cafes in Cornwall helping people manage pain without painkillers, relying instead on exercise and psychological support. Dependency on antidepressants has been shown to cause more harm than good (as anyone who watches Happy Valley already knows). Time to kick the diazepam.
Increasing awareness of the benefits of phytonutrients (the kind of stuff the health food industry has been emphasising for decades) is filtering through to the medical industry and impacting on social prescribing. It was the Dutch philosopher Desiderius Erasmus who famously said 500 years ago: “Prevention is better than cure.” With life expectancy rates going backwards, increasing rates of alcohol and drug-related deaths and hospitalisations, along with record levels of obesity, social prescribing is happening just in time. Will people be taking their prescriptions into the health food store? Or will the pharmacies try to capture this newly lucrative business?
The Bromley by Bow Centre in East London is pioneering the ‘new’ approach to health and wellbeing, and it is a model that is being emulated in more and more places.
Yes, the first reaction is ‘I told you so’ - but the fact is that these people are serious. At least so far.
How long will it be before doctors prescribe yoga and pilates classes or give out free prescriptions for herbal medicines and supplements? Will you get free cookery classes on the NHS?
There’s still a long way to go, but at least the direction of travel has finally changed. The Government has just allocated £50 million to support 42 Integrated Care Boards across the country to help doctors to ‘de-prescribe’ their patients and get them on the path to wellness without drugs. There will need to be proper support for the medical profession - they know it makes sense but it’s a steep learning curve for many doctors. They didn’t teach this kind of stuff at medical school.